From Rehab to Resilience: Sports Manual Therapy, Mechanotherapy, and Return-to-Play Success
Rehab doesn’t end when symptoms fade. In this article, you’ll learn how to use sports manual therapy, mechanotherapy, and progressive training models to help athletes recover faster and return to play with lasting resilience.
September 23, 2025
8 min. read

As a clinician, you’ve probably seen it: athletes trapped in rigid rehab protocols, immobilized longer than necessary, and frustrated when their recovery stalls. Too often, traditional models either oversimplify complex tissue demands or rush athletes back into strength and conditioning before foundational healing has occurred.
What if you could move beyond “technician-style” care and instead guide your athletes with an individualized, tissue-based approach that accelerates resilience?
In this article, we’ll explore core strategies rooted in sports manual therapy, mechanotherapy, and performance science—while showing you how to integrate them into practice. By shifting your perspective and refining your approach, you can help athletes not only return to play but stay there, stronger and more resilient than before.
Moving beyond protocols
If you’ve ever felt like a “technician” in your clinic—handing out the same exercises for every knee, shoulder, or ankle—you’re not alone. Early in my career, I relied too heavily on protocols. I knew the timelines, sets, and reps, but I didn’t always know how those interventions affected the specific tissue in front of me.
That’s where I began to shift from a technician to a clinician. Instead of thinking in terms of generic protocols, I learned to combine two critical models:
Pathoanatomical model: What’s the exact tissue involved? Is it a tendon, ligament, capsule, disc, or cartilage?
Impairment model: What functional deficits (weakness, motor control issues, maladaptive patterns) limit performance or delay healing?
The truth is, your athletes often need both. A post-op ACL demands tissue-specific loading, but your athlete won't regain stability if you miss the hip and core impairments. A healthy athlete might not present with pathology at all, but if you uncover mobility restrictions or motor control deficits, you can still improve their performance.
I often explain this to athletes using the metaphor of hardware, software, and fuel. Hardware refers to biomechanics, including joints, ligaments, and tissue structures. Software represents the neurological system, such as motor control, proprioception, and pain sensitization. Fuel is the biochemical side, including circulation, inflammation, and energy systems. If you focus on only one of these areas, you risk missing the real drivers of performance and healing.
And remember, you're never treating just tissue. You're treating a whole person influenced by psychology, environment, and social pressures—what we often call the biopsychosocial model. A coach who pushes a player back too soon, a parent worried about safety, or an athlete with fear-avoidant beliefs can derail the best rehab plan.
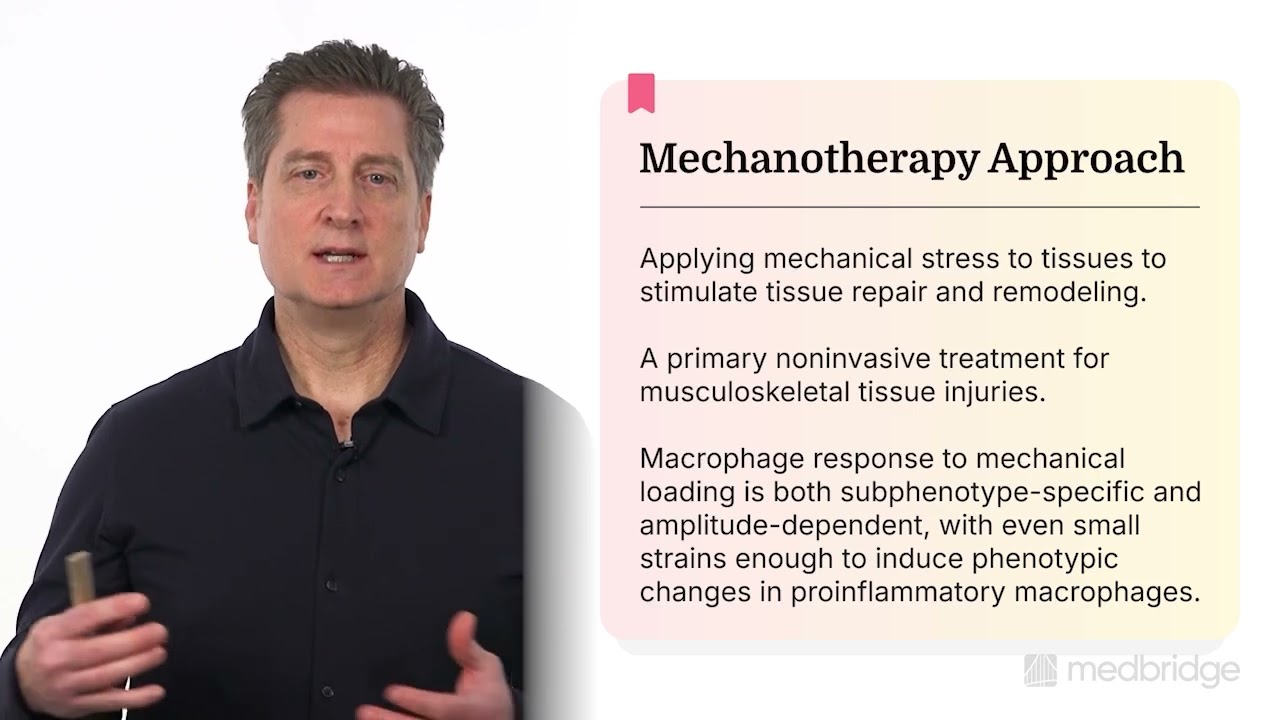
Mechanotherapy: Movement as medicine
The truth is, motion is essential for healing. Prolonged immobilization weakens tissue, reduces lubrication, and delays healing. If your athletes are stuck in boots, braces, or slings for too long, you’re not protecting them—you’re holding them back.
This is where mechanotherapy comes in. Mechanotherapy uses controlled mechanical stress to stimulate cellular repair and remodeling. It’s one of the most effective noninvasive treatments we have for musculoskeletal tissue injuries.1 Even small, well-dosed strains are enough to activate macrophages and fibroblasts, shifting them into a repair mode that accelerates healing.2
There are two main ways I apply mechanotherapy in practice:
Tissue repair training: In the acute or subacute phase, I prescribe low-load, high-repetition movement to promote lubrication, collagen synthesis, and early repair.
Tissue tolerance training: As athletes progress, tendon issues may require heavier, slower concentric and eccentric loading to build resilience and prepare tissues for the demands of sport. Cartilage, bone, and discs require progressive loading, including higher-intensity impact loading.
The critical piece here is specificity. A meniscal lesion won’t respond the same way as a tendon repair. A disc injury has different needs than a stress fracture. If you don’t know the tissue, you can’t match the optimal stimulus for repair (OSR) to activate cells in that tissue.3
That’s why I emphasize differential diagnosis. Even if you can’t pinpoint the exact tissue in lesion, you should be able to distinguish whether the problem is primarily one of compression or tension. From there, you can dose your interventions accordingly with progressive tension or loading throughout the full functional range.
The three buckets of training
Another mistake I see clinicians make is blending rehabilitation with strength and conditioning. These are not the same thing, and confusing the two often leads to setbacks.
I like to think in terms of three buckets:
Rehabilitation: Tissue repair, joint mobility, edema resolution, vascular stimulation, motor control, and early collagen loading.
Strength and conditioning: Hypertrophy, endurance, coordination, and osteokinematic strength.
Return-to-play: Agility, speed, power, sport-specific skills, and competition readiness.
When you keep these buckets distinct in your exercise dosage and design, you can meet your athletes where they are. Skip the rehab bucket, and you risk reinjury. Keep them in rehab too long, and you hold back their performance. Your job is to know when—and how—to move them forward. Research on collagen stress-strain behavior reinforces this need for progression, showing that tissue adaptation depends on precise, phase-specific loading strategies.4
Clinical example: Rethinking the ankle sprain
Let me give you an example. Years ago, I worked with a collegiate soccer player who came in with a lateral ankle sprain. The initial recommendation elsewhere was a rigid RICE protocol (rest, ice, compression, and elevation) and a boot for three weeks. By the time she returned to training, she had significant stiffness, poor motor control, and a fear of cutting. Within two months, she reinjured the ankle.
In my clinic, I took a different approach:
First 48 hours: Manage swelling, then introduce gentle, repetitive movements to stimulate collagen repair, reduce inflammation through venous pumping, and reduce pain.
Rehabilitation bucket: Restore the axis of motion in stiff joints in the biomechanical chain (e.g., the subtalar and calcaneocuboid joints), train for increasing local vascular supply and proprioception, and increase muscle spindle sensitivity to stretch in the muscles of eversion to support damaged collagen and impaired mechanoreceptor feedback.
Strength and conditioning bucket: Add eccentric peroneal training, proximal trunk and hip strengthening, and progressing into load-bearing drills.
Return-to-play bucket: Integrate cutting, reactive balance, and sport-specific agility challenges.
She returned to competition sooner and with more confidence than she would have under a strict immobilization protocol. Most importantly, she stayed healthy throughout the season.
What this approach means for you
As a clinician, you’ve probably faced the tension between cautious protocols and athletes eager to return to play. My advice: don’t let protocols dictate your care. Use them as a guide, but always come back to the tissue in front of you.
Sports manual therapy gives you the tools to blend pathoanatomical precision with impairment-based reasoning. Mechanotherapy provides the science and structure to load tissues safely and effectively. And the three-bucket model ensures you’re progressing athletes logically, without skipping steps.
When you practice this way, you stop functioning as a technician who hands out generic programs. You become a clinician who thinks critically, adapts dynamically, and transforms outcomes.
From rehab to resilience
Over the years, I’ve come to see resilience as the true goal of rehab. Any therapist can get an athlete back on the field. The real question is: will they stay there?
If you integrate sports manual therapy, mechanotherapy, and the three-bucket model into your daily practice, you’ll help athletes heal and develop the capacity to withstand the demands of their sport. You’ll refine what you already know, add specificity where it’s missing, and differentiate yourself as a clinician in a crowded field. Most importantly, you’ll give your athletes the best possible chance not only to recover but also to thrive.
If you’d like to take a deeper dive into these concepts, I explore them in detail through my Medbridge course series:
Rehab to Resilience: Transforming Sports Therapy Outcomes – Integrate advanced sports manual therapy with tissue-specific rehab and performance optimization.
Tissue Repair Training in Rehabilitation and Athletic Performance – Apply mechanotherapy principles, exercise dosing, and differential diagnosis to bridge injury management and return-to-sport.
Seven Core Principles of Sports Manual Therapy – Strengthen your framework for mobility, motor control, and performance using evidence-based manual therapy.
Precise Loading: Optimizing Dosage for Tissue Repair and Rehabilitative Exercise – Design tissue-specific loading strategies that improve recovery and outcomes.
Advanced Tissue Training: Lower Extremity Tendon Pathologies – Use progressive loading and mechanotherapy to safely rehab Achilles tendon injuries.
Patellar and Hamstring Injury: Optimizing Collagen Tissue Health – Refine your approach to patellar and hamstring tendinopathy with advanced rehab strategies.
Advanced Tissue Training: Upper Extremity Tendon Pathologies – Explore evidence-based care for lateral epicondylalgia and rotator cuff pathologies.
References
Seo, B. R., & Mooney, D. J. (2022). Recent and Future Strategies of Mechanotherapy for Tissue Regenerative Rehabilitation. ACS biomaterials science & engineering, 8(11), 4639–4642. https://pubmed.ncbi.nlm.nih.gov/35133789/
Babaniamansour, P., Jacho, D., Teow, A., Rabino, A., Garcia-Mata, R., & Yildirim-Ayan, E. (2024). Macrophage Mechano-Responsiveness Within Three-Dimensional Tissue Matrix upon Mechanotherapy-Associated Strains. Tissue engineering. Part A, 30(7-8), 314–329. https://pubmed.ncbi.nlm.nih.gov/37725574/
Rivard, J., & Grimsby, O. (2008). Scientific therapeutic exercise progressions (STEP): The lumbar and lower extremity (1st ed., Vol. 3). The Academy of Graduate Physical Therapy, Inc.
Wohlgemuth, R. P., Sriram, S., Henricson, K. E., Dinh, D. T., Brashear, S. E., & Smith, L. R. (2024). Strain-dependent dynamic re-alignment of collagen fibers in skeletal muscle extracellular matrix. Acta biomaterialia, 187, 227–241. https://pubmed.ncbi.nlm.nih.gov/39209134/
Below, watch Jim Rivard discuss mechanotherapy in this brief clip from his Medbridge course "Rehab to Resilience: Transforming Sports Therapy Outcomes."